Hi guys!

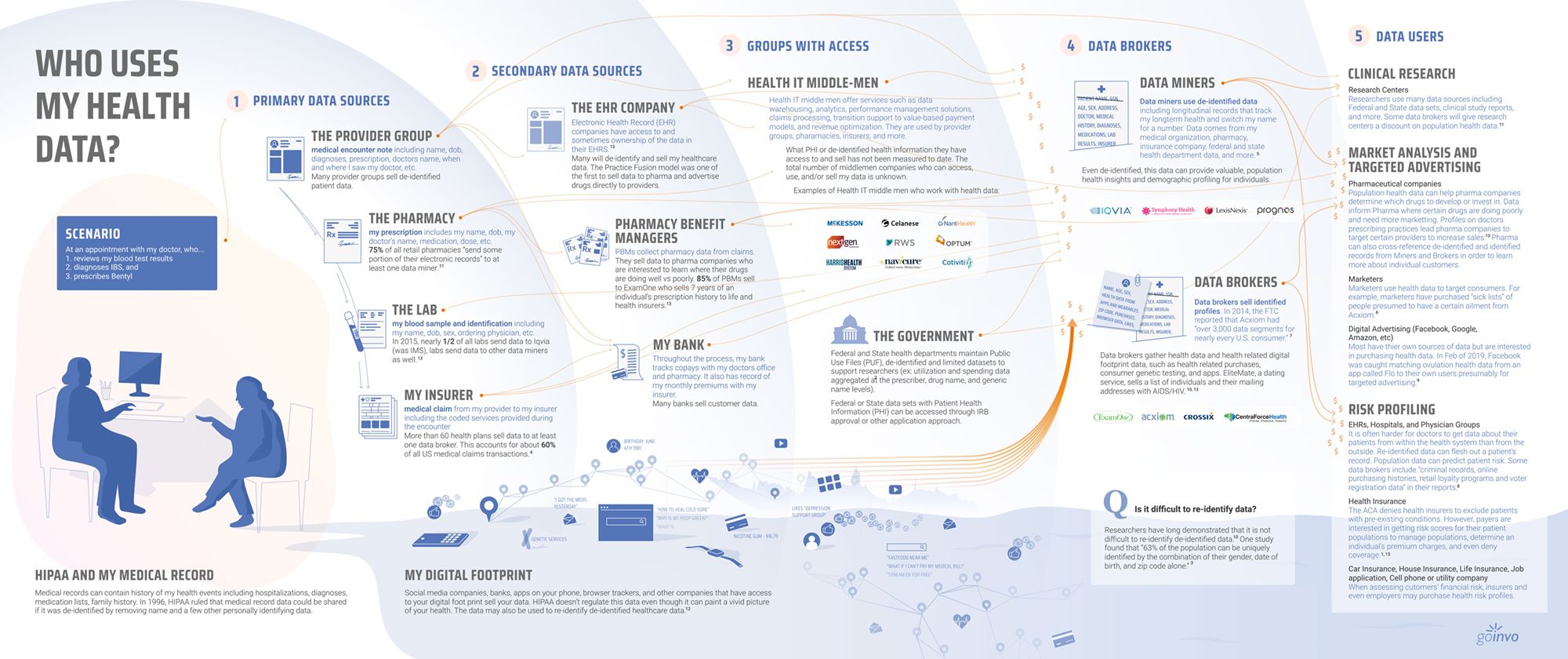
So I wanted to check-in. I knew technology in healthcare was going to be well…crazy when big business got their hands in it but yikes! I know some of my patients have been getting the new “check-in” links which is great as a clinician, but I have some GIANT concerns with where healthcare is headed without CLINICIANS leading the charge. I am already getting a TON of patients reading the technology agreement by one of the “HEALTHCARE PARTNERS” I was recommended by my EHR; and they are not happy about “signing away their HIPAA rights and healthcare data being sold”. I looked at some of the terminologies and could see immediately what some of my patients were quite upset about. They were not happy that there was the potential of “targeted ads, and other such things based on the technology agreement they had to sign with the technology company that owns the platform doing my patient check-ins…one told me she was offered a magazine subscription that it was made to look like it was from me, the clinician…and furthermore it made it sound like I was going to get paid for it.”
Now, while everyone who knows me, knows that I am a significant advocate for having things tailored based on patient needs… if companies start applying AI (artificial intelligence) without having the provider in direct control of these items that are being presented to a patient based on “health scores etc.” or “health information” and all based on AI that really doesn’t know the patient is highly dangerous. It is dangerous for medical patients, and it is even more dangerous in a psychiatric setting. I have many partners that I work with, but the clinician is ALWAYS in charge of anything that is recommended to a patient when it comes to health-related information.
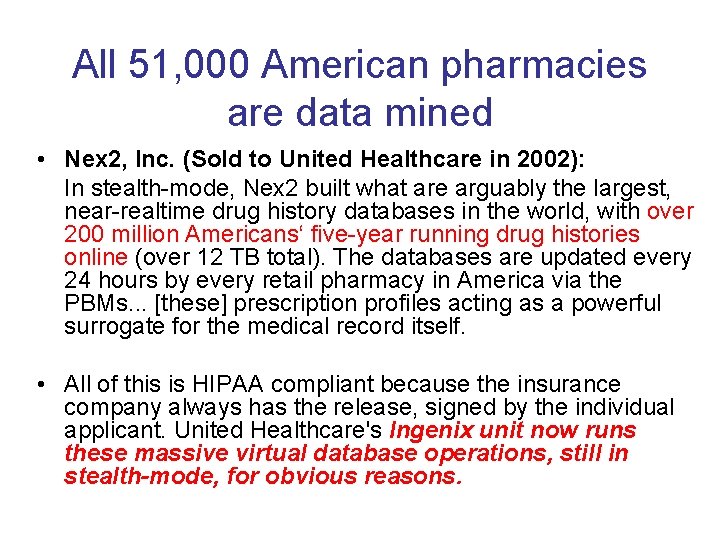
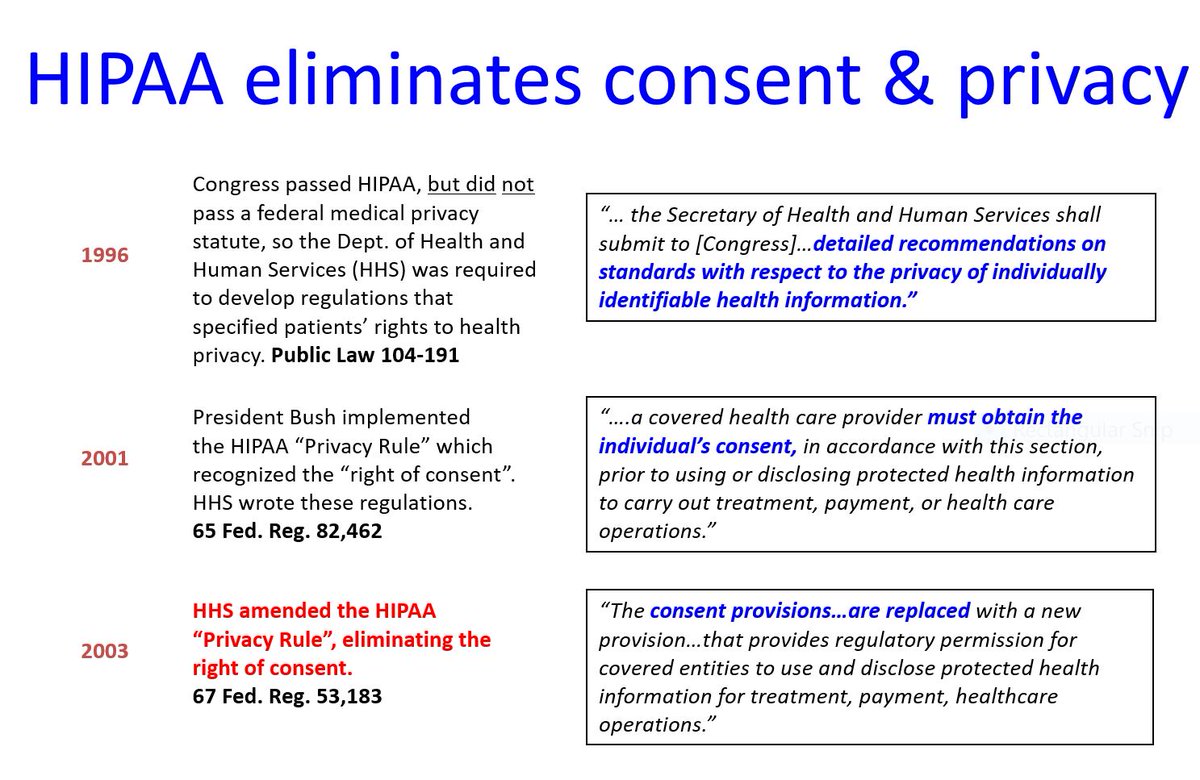
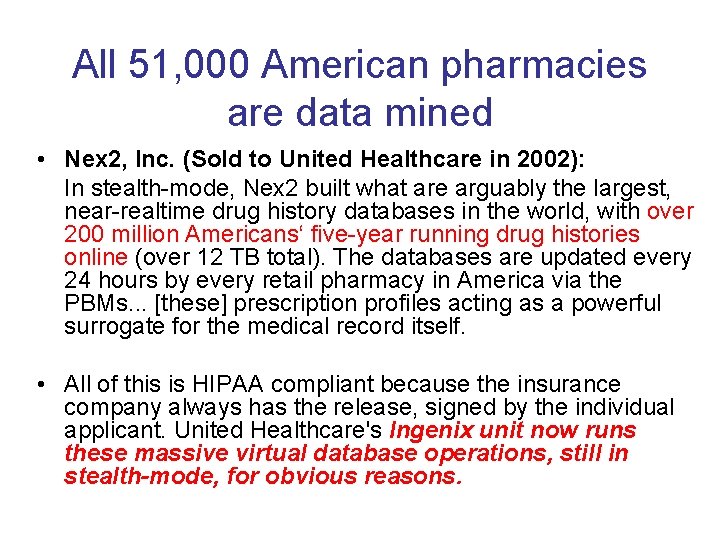
What I am finding now though, as more tech companies have decided that healthcare technology is where they can be super lucrative, the same tech nerds that brought us the social dilemma 1.0 are now quickly headed into doing the same with our healthcare data. They are basically having patients sign consents that allow the tech company to use their PHI that they are collecting for their doctor, and using that to target ads. This technology assumes that the person “signing” the technology consent is able to actually competently sign to receive “targeted information”. However, even if a patient felt they were able to do so, health information is highly sensitive, behavioral health records even more so, and even if you say target depression with a “depression related app offering” because of say in theory a PHQ-9 score, or a chart diagnosis you thought you had comes to you, that in no way implies that it is the correct intervention for a patient, especially if it is not evidenced-based. That is a phenomenal way to end up with a DEAD patient. I can’t tell you how many people confuse WHAT TYPE of DEPRESSION they have. Let’s say you end up with targeted ads for an intervention for “DEPRESSION” that one day is harmful for BIPOLAR DEPRESSION. IF these dumb AI robots give you an intervention for DEPRESSION that could kill someone with BIPOLAR DEPRESSION, who accepts the responsibility? Well, it sure as heck isn’t the tech company is it, they put the risk on the patient, who signed away their “HIPAA RIGHTS”, which they had to do in order to access me the clinician (on their EHR, or through TELEHEALTH, or on their healthcare app). They had to sign this consent so they can be given targeted ads, potentially on a wrong diagnosis they might have typed in, and all in the name of business while claiming, “well we told you we weren’t healthcare providers”. Did you? Did you really? (sarcasm).

The answer. No, they didn’t. This is no true “informed consent” procedure that is up to healthcare standards for this technology. There is no assessment to ensure the person on the other end is actually understanding the information they are being presented. This is no different that CELL PHONE COMPANY DEVELOPER X, making you sign the 20-page agreement that no one on earth has time to read, and even if we do read the small print…can anyone truly and easily operate today without their cell phone that will die after 2 years of mandatory updating? Not really…and now they are going to cut off access to your clinician too, by having you sign a billion-page document, that ultimately is signing your HIPAA rights away so they can maximize profits! Half the time the clinician will be none the wiser. I had an inkling this would transpire eventually, but I wasn’t even aware until a patient sent me the first concern. (because my agreement and what the patient signs are two VERY SEPARATE agreements).
As you all know I am also highly involved with pharmacogenomics, genetics, genomics etc. This is another area where many companies like 23&me and even other companies with tighter FDA regulations in my opinion are going to find themselves in very murky waters when offering patients very inappropriate (what should be considered treatments and interventions) based on healthcare-related data. This is NOT AT ALL the same as google clicks and hand-feeding you political articles making you feel like you are in the majority of believers, even if you are a small minority with targeting google searches and clickbait ads…we are talking now about interventions that are going to be applied to A PERSON’S LIFE based on HEALTHCARE DATA. This is not giving you a Twitter feed full of people with similar viewpoints to yourself based on what you are Tweeting, Tweetbotting, or whatever TWIT platform is being used by the end-user today… this is a person’s LIFE, HEALTH, and BASIC HUMAN RIGHT here.
We already know that most conditions are polygenetic, many have epigenetic triggers, and you cannot correlate a single gene to disease in most cases. (Yes I am aware there are some diseases with a single gene). You CAN however create a risk score based on polygenetic risk etc.) But even with all the genetic data it is still not and NEVER WILL BE a certain correlation…psychiatry is the perfect example. You still need to know which you will only get from epigenetic considerations. I have patients with ALL The RISK GENES (or major ones identified thus far) for bipolar disorder. IN fact, I see this frequently in children. But when they are given the right structure, stress is kept low, healthy diet, (and basically never given any epigenetic triggers ever) they NEVER present with a clinical issue. Why? Well simple. No epigenetic triggers. Substance use is another example. Even if we figure out ALL the substance use genes, I have PLENTY of clients who because their entire family was a substance user they opted to never touch the stuff and no epigenetic trigger. I had others that DID touch the stuff, just to see…and guess what, they didn’t suddenly have substance use disorder either. Their epigenetics pushed so hard in the opposite direction and probably with a hot and heavy sprinkle of resiliency genes; and they never ended up struggling with SUD. If you can show me the AI that can calculate all that, like what my brain does naturally at this moment (sometimes I swear it is the only thing my ASPIE INTJ brain is for), by all means, SIGN ME UP yesterday. But I can tell you it doesn’t exist. AMAZON & GOOGLE may have the power to track the data, but to be able to apply population medicine to an individual at this juncture, clinicians aren’t even half the time successful at it. Or I highly suspect we wouldn’t be having to educate clinicians on the nuance between ruling out a Bipolar depression vs. Major Depression, and which treatment to offer.
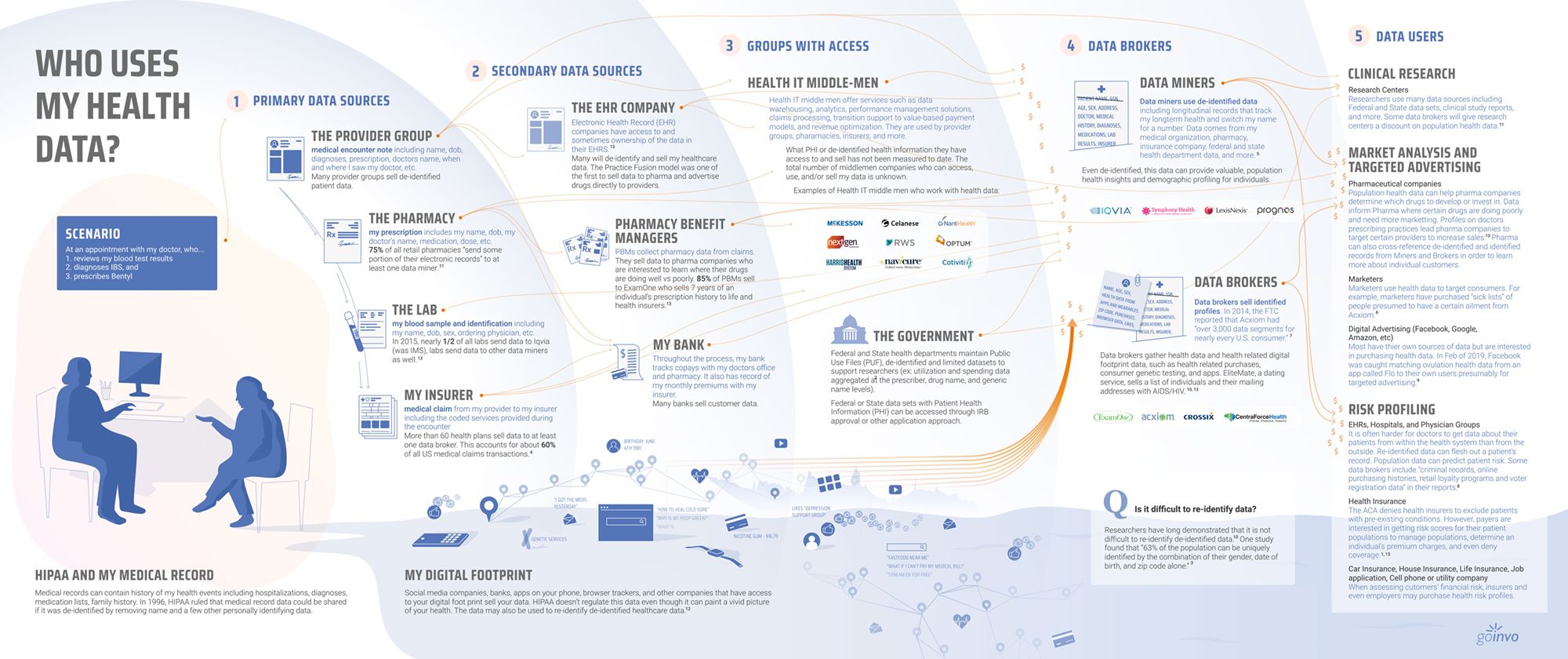
https://www.goinvo.com/vision/who-uses-my-health-data/
Do you know how many patients I have had that have gone home to try and commit suicide because healthcare TRAINED professionals offered up a fibromyalgia diagnosis in an ER for their chronic pain-related issues, and told them that this condition was not really able to easily be treated? I can tell you it is more than 1, which is already 1 too many. The last thing I want, is some AI delivered “depression magazine” or other non – provider approved intervention, to be given to someone who already feels isolated and alone, based on AI technology by some tech developer, who developed some robot algorithm, who can profit from patients and their healthcare data, using non-medical approved intervention, but using anything that, me as the clinician, even remotely appears to come from me — when I am the one with the license, the malpractice, and everything to lose. I also don’t want to lose a patient’s life to an intervention that may be highly inappropriate for them because of said AI robot that is brought to you by tech giant A or corporation G or social media platform F applying any population-based medicine to an individual with individual health needs that were not considered.
I will also point out that “evidenced-based” interventions even at their best are sometimes only effective for 60% and can still be “statistically significant”. Many drug treatments with FDA approval only ride at the 30% effectiveness or less, as indicated by the STAR*D studies and other such literature reviews and significant healthcare studies. Does that mean every clinician only meets a 30% efficacy with the patient? No, we don’t, why, because we factor in individual needs when considering this literature. But, if you only apply the evidenced-based literature, What about the other 40% or 70%? Are they just going to be screwed, or forced to have some side effect? Or worse, end up dead from some AI robot intervention that didn’t consider the individual in front of them?
There are many ways to arrive at the statistical significance and it is not always by helping the “majority”. I was exceptionally worried about individuals who are not clinicians starting to control these applications, with absolutely NO MEDICAL background. And while you may legally be protected as TECH GIANT xyz legal corporation agreements, by offering something a patient signs, my job as a clinician is to advocate on behalf of the patient to ensure that optimal outcomes are achieved. By implementing technology, based on AI with a signature, tech developers may feel that it is justified, but in my opinion, the patient needs to be working with their doctors/nurses/other healthcare professionals that work with them directly when it comes to offering any such “targeted” ads, apps, clickbait or anything else when it concerns health data.
I have discussed how HEALTHCARE INSURANCE COMPANY nurses…read a file, look at documents, but they don’t have any relationship with the patient and this can be just as problematic. INSURANCE GIANTS have also started to “target interventions…and mind you, at least those are evidence-based” but they are still failing and costing the system by blanket targeting these interventions that are not relevant to many patients. Their “cost savings” measures that are applied in psychiatry, I can tell you, for a start, are some of the most ridiculous and expensive I have ever seen. If they were truly following “evidence-based practice” to perfection, we would not have a single readmission hospitalization within 30 days paid for by any insurance company where a patient with schizophrenia wasn’t placed on an injectable dopamine receptor blocking agent (formerly known as an antipsychotic). The literature time and time again support they are the most cost-effective and stabilizing treatment to date in schizophrenia, yet this is not what is applied in the U.S. Only a fraction of patients are placed on injectable medications even though health practitioners in psych/mental health are hammered over the head with how these should be first-line for psychosis. But, half of the insurance companies have applied “cost savings measures” that make it impossible to get a patient a “clean injectable” that isn’t straight out of the 1960s treatment book because they look at “cost” first but didn’t calculate all the expenses on the back end associated with metabolic syndrome, endocrine dysfunction (which by the way exacerbates psychosis) and if you give that risperidone or Haloperidol deconate, you may be shooting yourself in the foot to stop those hallucinations and causing 16 other inappropriate hospitalizations for obesity-related complications, hirsutism, prolactinomas etc. Test after test will be run all because to “save money” a clinician was forced to offer haloperidol deconate over say an aripiprazole injectable. To which I get to write joyous and long letters (sarcasm) just like this to said insurance provider, to appeal to a non-clinician on a computer prompter of why my patient should have a treatment which most assuredly in the long term would cost the least amount to society. Which is a giant waste of everyone’s time, and if I am lucky will get said intervention approved before they are in the hospital AGAIN because I was too busy appealing what evidence had already supported as the most efficacious treatment, plus already known to have less long term risks than the other medications I am forced to consider that NEVER take individual concerns of my patient that I have treated usually for YEARS into consideration. Plus, let’s just go ahead and look at the hospital systems themselves. After all most of them are owned by an MBA. Basically you have another entity that only stands to profit off the patient being sick. So our poor patients with schizophrenia, even when FREE INJECTABLES from the pharmaceutical companies are offered to them just like any other clinician are never used and gather dust on the shelves because the hospital system touts A) that they don’t believe in pharmaceutical company relationships – convenient … B) They make money off EVERY ADMISSION even if it is 2 days after discharge C) they make money of the generic pill that their pharmacy obtains and D) They make money when the nurse, the care manager, the clinical social worker, the community support worker, the therapist, and the hospital affiliated clinicians see this patient for having to keep said sick patient from “going inpatient” and keeping them on the chronic outpatient program. Not only that all of these facilities are given extra government funds to help “keep this patient well” by being a “community health center” because of how “expensive and costly they are”. When they are 100% contributing to the expense by not giving injectables, giving old drugs with adverse effects that their hospital pharmacy makes money on, and by underpaying yours truly, the nurses and one to one staff they are employing.
https://slidetodoc.com/cambridge-university-electronic-health-records-which-is-worse/
Another example of insurance trying to utilize their AI similarly, who I can tell you has been tracking data in healthcare longer than a general non-clinical AI developer TECH COMPANIES, and has clinicians on staff as medical directors; I have a patient that received for example a “screening kit” for colon cancer from A VERY LARGE INSURER, less than one month after she had a full colonoscopy.” And while I, the clinician, in this case, would have still encouraged the patient to still do the kit because a biopsy may not have been completed, or something could have been missed on that exam…this patient was quite upset that she was being “harassed by a nurse she didn’t know, about a kit that didn’t make sense to her”, and “her doctor” (meaning me the APRN treating her) “was not consulted”, and then furthermore the INSURANCE COMPANY CHRONIC CARE NURSE couldn’t explain why this scan was important and necessary. All of which are GIANT and important factors when delivering QUALITY CARE. (As a reminder the United States has some of the most expensive and the worst health outcomes for first world nations). For those of you I have taught to research this…don’t compare on the zebra diagnoses. It is silly to compare the U.S. on autoimmune to Japan when there are more cases of autoimmune in the U.S. You need to try to compare oranges to oranges. So one of those instances is maternal-fetal outcomes. Women are given birth to babies EVERYWHERE. IT is routine. United States outcomes, mind you where the majority of us are cared for in the HOSPITAL, are the HORRIFYING! Here is a nice little synopsis: https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries
Back to our client with the poop test. This client had already told the nurse to screw off, that she (the nurse) knew nothing about her (which was true) outside of the “health collected data supplied by the insurance company, and diagnoses on her chart”. This nurse didn’t confer with me, this was a “blanket evidence-based approach without any thought”. Now, I’m not going to lie, I have a little bit of stronger invested interest in this, as I supplied said insurance company some strong evidence for how to do a chronic care management program.
Evidence-based medicine is not blanket applying treatments because some study, even if it is a Cochrane literature review, says that there is statistical significance in offering an intervention; (although it is frequently misconstrued as such especially when someone stands to profit) — it is understanding the evidence as presented and then requires someone with some medical knowledge to interpret whether that “rule” or that “evidence” is in the best interest of the individual in front of them (unless said data clearly shows that 100% of people given the treatment improve, offering it as a blanket treatment will end up costing on the back end)…which last I checked still took a healthcare degree and had a direct working relationship with the patient. If you just apply even one singular evidence-based medicine intervention to the population, you are still only treating health at the population level and not the individual level. It is costly in lives and money. A clinician is trained to be considering both the population and the individual, and weighing those options before selecting what would be the best interventions for a patient is 100% still necessary even with a robot offering up CLINICAL DECISIONS.
There is NO WAY that the AI currently being developed in healthcare is ready to pull out the necessary data in order to be able to then interpret and analyze from multiple selections of the best interventions for a client. I will give you another example. In medicine, a beta-blocker may not be first-line for a patient with HTN. In fact the current hypertension guidelines, it is not. But a smart clinician may be able to see that a beta-blocker would, by all means, be the best treatment for someone who has mitral valve regurgitation, panic attacks with social anxiety, hypertension, and tachycardia. This would be a MUCH BETTER first-line agent in all likelihood for that patient (over diuretic + our ACE/ARB) pending there aren’t other factors like asthma which would then require a knowledge that perhaps nebivolol in the UK is used in congestive heart failure (CHF) and has evidence to support that it doesn’t exacerbate pulmonary related symptoms. OR that perhaps they may need to look at alternate treatment. Yes, this is a medication, but other offerings that seem even as “benign” as a magazine can have disastrous outcomes for a patient. In addition, a patient may refuse medical care, but they are NOT the most informed when it comes to knowing if the interventions being targeted at them are going to be helpful or harmful for their condition. I tell my patients ALL THE TIME not to beat themselves up for not knowing something was good or not for their health. They didn’t go to school for the inordinate and amount of time that I did with record second mortgage creating debt that I am in to become a healthcare practitioner. Patients choose FAST FOOD every day, and in nursing, I like to consider that to be a “SIGNIFICANT KNOWLEDGE DEFICIT” because where people may have learned that “FAST FOOD is bad for them”…do they know why? I mean with a strong, INFORMED, and significant understanding of what that is doing to their body and in relation to their personal illnesses”? The answer is No. (For those that might still be wondering). Patients generally do not know why fast food is bad for them and their personal health condition. So these piddly “technology consents” that the business technology giant powers-that-be, that make all the money, have slapped together to cover their butts, are by no means a protective measure for patients and in NO WAY an INFORMED CONSENT MEASURE.
I have over and over advocated how technology can be a great asset in healthcare when applied appropriately. But if any technology entity is applying, offering treatments and interventions, magazines, or other literature without a directed healthcare professional approving these products, that in my opinion is 100% practicing medicine without a medical degree — or RN even”. It is in no way shape or form appropriate to target any sort of offering to a patient whether it even be an unrelated health magazine. If that data is obtained from a medical record or informational system that comes from their health record, or even clicks based on a clinical encounter, the patient needs to be protected from their data being exploited. HECK! I’m A PATIENT TOO AND I WANT TO BE PROTECTED!
HEY AMAZON, I am talking to you, because I’m here trying to REVOLUTIONIZE healthcare over here for the better, and if you want to avoid “The Social Dilemma 2.0”, BEZOS, CALL ME–let’s make this happen the right way! There is a way to do this — without exploiting humans! 😉
I want to ensure that my patients are safe, that they are being offered valuable healthcare interventions. If it has ANYTHING to do with their health-related clicks. Or even more sensitively based off a PHQ-9 score, or even more sensitive a diagnosis or one step farther, someone’s GENETICS etc., then you cannot cut me, the clinician out of things when I have been here, on the ground with the patient for ten years and know them sometimes better than my own family (from being overworked by this system called healthcare as we know it!).
I just want to ensure that any “targeted ads, AI, or other technology being recommended to my patients is appropriate” and would not cause further damage and worsening outcomes to their health.
I also know that as a clinician, for most of these technologies, I am significantly overpaying you to utilize said technology in my practice. Then you are turning around and making a second profit on now targeting them like you have some kind of special healthcare knowledge because I introduced you into my practice!!! Then when your little tech waiver suggests that I am possibly making a profit from the technology or the magazines or whatever other clickbait you are providing so you can slip in there that you may be profiting too…HEY TECH PEOPLE, I’M TALKING TO YOU! I CAN’T GET PAID THAT WAY ding dongs (actually I know you know this which is why it isn’t mentioned in my BAA to you that you are going to do this to my patients)…because the rest of the world knows ALL YOU MBAs tied my hands YEARS AGO. I can’t make a profit of their health or their health data because of Anti-kick back statutes. So stop telling my patients that you are “paying me” or that I might be getting any sort of “reimbursement” for these targeted CLICKBAIT bogus interventions or for any sort of intervention that is being offered to my patient. The data they are clicking when checking in with me for telemedicine, or into their medical portal, or in any other medical app I am utilizing, should in no way shape, or form be used to offer “click ads for antidepressants, or click ads for a medical device, or click ads for an app” without express approval from the provider who is actually THE TREATING PROVIDER. But I know that is why you didn’t tell me in my BAA because you all knew that I will NEVER sign some blanket waiver for technology whether an APP or an EHR, to just offer things carte blanche to a single one of my patients without strong evidence that it is in the best interest of my patient.
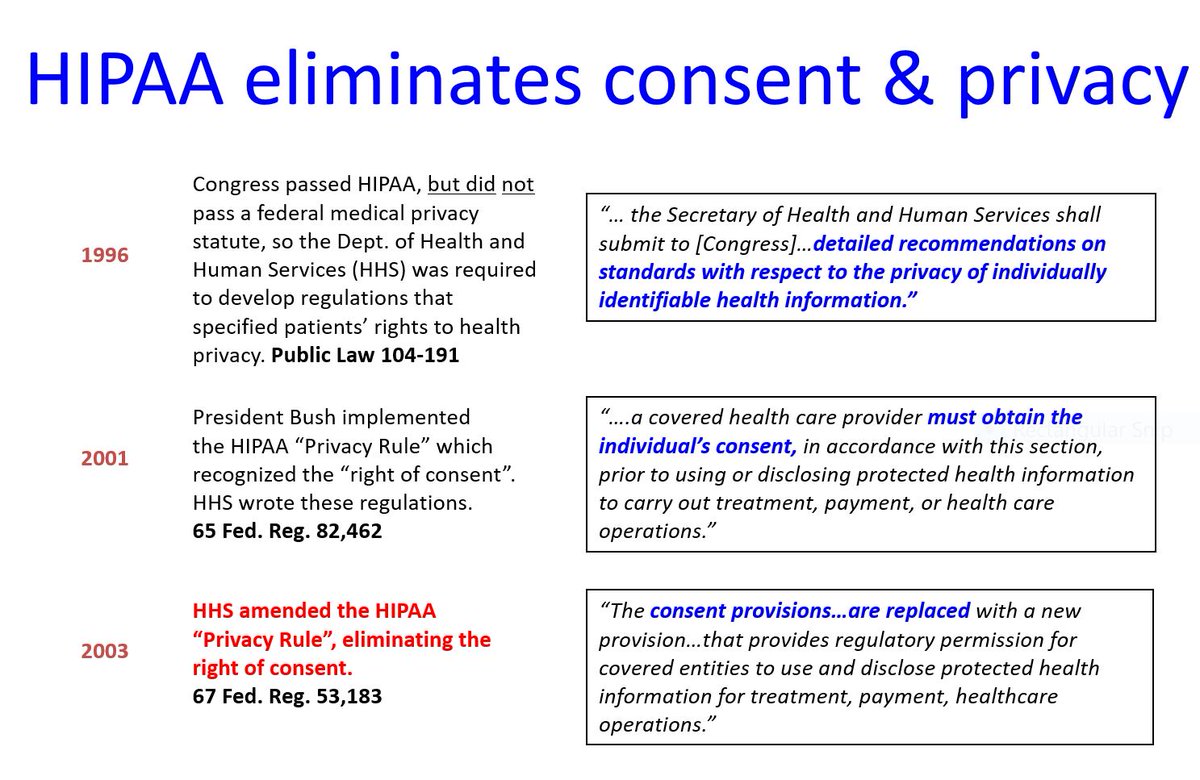
So US Government, so FDA, so MEDICARE, and OIG, the ball is in your court! Because the tech community has started this game. It is on you to protect the patient now because you stripped my power a long time ago as a provider. Are you going to hold them to the same ridiculous standards as I am? Are they going to have to pay thousands for each of their providers in CEUs, are they going to have 200,000 in debt for 10 years of education, are they going to have to pay for malpractice, are they going to be liable for all the kickbacks they receive for offering Apps to patients by their PHI? Or are these pretty little technology waivers enough to absolve them of any risk whatsoever to offer a product to a patient based on their medical communication to me, the provider, overworked by this CORPORATE PRACTICE of MEDICINE because they got someone to sign a document that says now their data is no longer “HEALTHCARE data” and snuck that in the fine print? Are they going to be held accountable for not supplying true medical informed consent with all the training that entails? Please, let me know because if this is the future of healthcare as we know it, because if it is…. I’m out! The exploitation was bad enough before TECH companies “mining” our “PHI” that is no longer “PHI because we signed saying it wasn’t”!
So TECH GIANTS, as a customer who has been forced to paying exorbitant prices for years because it was “healthcare technology”, and on behalf of my clients; I want you all to be held to my standards to offer “HEALTHCARE interventions”. You with your MBA, running health care, you who hijacked the hospitals years ago, you who took over with the insurance companies, I do not want YOUR BUSINESS DEGREE MBA from an online community college to target my patients based on any HEALTHCARE data clicks, uploads, or shares. I DO NOT WANT, your non scientifically proven apps, treatments, or magazines offered to my PATIENTS (my patients who are living breathing humans with families, and parents, and siblings!). My patients and every single one of US is a PATIENT at some point! You are in NO WAY SHAPE, OR FORM QUALIFIED to make any decision of what to offer my client in your clickbait! You should not be allowed to charge me exorbitant prices and then turn around and gouge my patients on your click ads! While I, the clinician, have to pay for all the risks. I have to pay for cyber protection of their data. I the covered entity have to pay for coverage for your healthcare data breaches! And the government already took away my ability to make money on any intervention offered to a patient years ago, but why are you allowed, tech person with MBA allowed to make all the money of their data and you know nothing about them?
If I am not directly approving the interventions themselves, plus NOT being provided all this data you have gathered and “mined”, that really should have been given to be plus a steak dinner and a TESLA because of your overpriced technology listed as “Healthcare Technology”; I do not in any way shape or form as the clinician and as a nurse as well; approve of any intervention being applied to my patient without them being fully informed BY YOU THE PROFITER unless you are using a full MEDICAL INFORMED CONSENT processes, of the interventions (that is what your clickbait, apps, target at health really are) without them being fully aware of all the risks vs. benefits of any said intervention. This includes all your apps, magazines, technologies, link to other services, links to treatment facilities, links to educational organizations, or any other such treatment or intervention that you all may view as “marketing”. In reality, once has been offered based on your “mined” health information and the PHI you have collected from my practice, it ceases to be marketing and is now 100% is “interventional”. If I give a scrap of paper with directions on it, I as a healthcare professional can be held accountable. Well, you know what tech companies, you can’t just take my patient’s health data, have them sign a little slip of paper that says they allow you to offer interventions, and not be held to the same standard that I the clinician am, and expect people to be okay with that. If you want those profits, then pay for it with the blood, sweat tears, malpractice, board certifications, and everything else I did. Not just because you took an advertising and coding class online. Try and figure out how to make a profit with a healthcare professional license LEGALLY while not exploiting the people you serve.
A nurse (RN) that identifies a patient at risk for breathing deficits and offers links to healthcare groups that can assist with breathing support is still supplying a “healthcare intervention” that is bound to their license. They can still be sued if the links they supplied resulted in worsening of the patient. But you TECH GIANT are allowed to do the same thing without a license, or sitting in the basement of your parents’ home and profit off me the clinician, AND my patient, where is the logic in that?